How To Become HIPAA Compliant
Become HIPAA compliant by understanding that HIPAA rules and regulations are often complex and difficult to interpret. They cover a wide range of requirements related to the privacy and security of protected health information (PHI), which can make compliance challenging.
Healthcare professionals responsible for HIPAA compliance must understand not only the law itself but also how it applies to day-to-day operations. This includes everything from handling patient data to securing electronic health records and managing third-party vendors.
Because of this complexity, many professionals feel overwhelmed when trying to ensure their organization stays compliant. Clear guidance, ongoing training, and practical tools can help simplify the process and reduce the risk of violations.
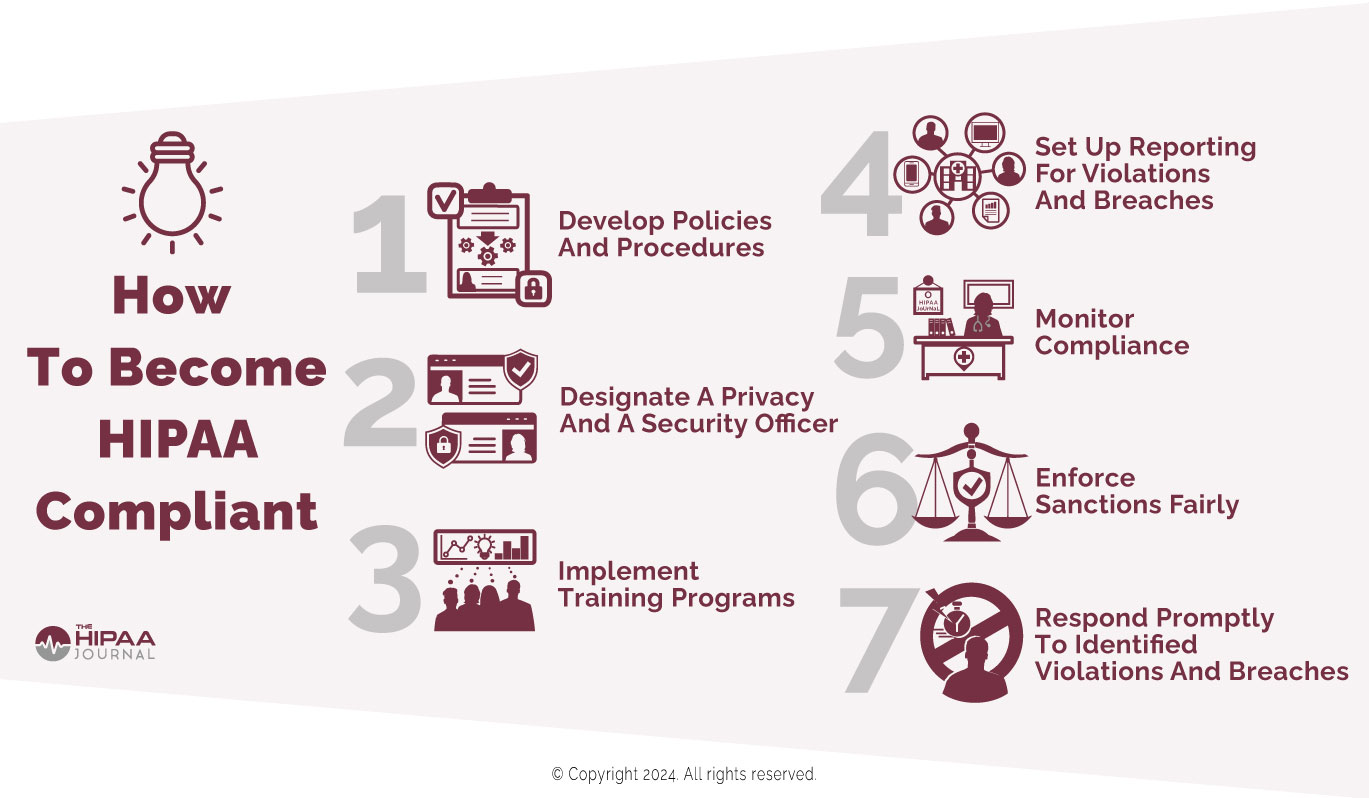
7 Steps for HIPAA Compliance
In 2011, HHS published “The Seven Fundamental Elements Of An Effective Compliance Program”. We have slightly amended it to be more relevant to HIPAA compliance in 2025. Here is a summary of the elements, which we outline in more detail in this guide.
- Develop policies and procedures so that day-to-day activities comply with the HIPAA Privacy Rule.
- Designate a privacy officer and a security officer.
- Implement effective training programs.
- Ensure channels of communication exist to report violations and breaches.
- Monitor compliance at floor level so poor compliance practices can be nipped in the bud.
- Enforce sanctions policies fairly and equally.
- Respond promptly to identified or reported violations, and breaches.
You can also read more about the background and history of the Seven Elements here. You might consider using HIPAA compliance software which has been designed to use the seven elements framework and can simplify and automate compliance, and provides comprehensive risk management processes.
Step 1: Why HIPAA Privacy Rule Policies and Procedures?
Although HIPAA compliance consists of complying with all relevant Administrative Simplification Regulations, implementing HIPAA Security Rule and Breach Notification standards is generally an organizational process not connected with cultivating a culture of compliance. Additionally, the most common HIPAA violations are attributable to failures to comply with the HIPAA Privacy Rule.
However, it is no longer sufficient to develop policies and procedures that only address permissible uses and disclosures, the minimum necessary standard, and patients’ rights. Covered entities should ensure HIPAA Privacy Rule policies and procedures include how to explain to patients what PHI is (and what it isn’t), how to verify an individual’s identity, and how to record requests for privacy protections.
Step 2: The Roles of HIPAA Compliance Officers
It is interesting that the HHS’ Office of Inspector General placed this “tip” in second place after the development of policies and procedures. This would imply the roles of HIPAA compliance officers are to train members of the workforce, monitor compliance, and enforce the organization’s sanctions policy. However, there is quite a lot more involved in being a compliance officer.
In most cases, the HIPAA Privacy Officer will be the point of contact for members of the public and members of the workforce that want to report privacy concerns. Security Officers are generally more responsible for conducting risk assessments, ensuring security solutions are configured properly, and training members of the workforce on how to use the solutions compliantly.
Step 3: What Makes an Effective Training Program?
The effectiveness of the training provided to members of the workforce can make the difference between ticking the box of compliance or cultivating a culture of compliance. To make HIPAA Privacy Rule training effective, members of the workforce must understand what PHI is, why it has to be protected, and the consequences to patients, employers, and themselves of HIPAA violations.
HIPAA Security Rule training must be focused on protecting PHI in all formats and even more focused on the consequences of taking shortcuts, circumnavigating safeguards, and failing to alert managers of a data breach for fear of “getting into trouble”. One way of achieving this is to ask members of the workforce to run personal online credentials through the HIBP database to illustrate the importance of unique, complex passwords.
Step 4: The Importance of Two-Way Communication
While policy making and training has to come from the top down, it is important that any channels of communication relating to HIPAA compliance are also bottom up – not only to raise compliance concerns or report HIPAA violations, but also to provide feedback on what works and what doesn’t on the ground floor, and what new challenges are facing frontline members of the workforce.
This is why it can be important – when resources allow – to have a compliance team consisting of team members that have worked in or have knowledge of how different departments operate. For example, a compliance team consisting solely of lawyers and IT managers may not appreciate the difficulty of protecting the privacy of PHI in front of a grieving family mourning a recent loss.
Step 5: How Most Poor Compliance Practices Develop
Most poor compliance practices result from well-meaning intentions – for example, to “get the job done” or provide a good service to a patient’s family. When minor violations are allowed to continue, poor compliance practices can develop into a culture of non-compliance. This is why it is important to identify and address poor compliance practices at the earliest opportunity.
While it is important to have eyes on compliance at floor level, it is also important not to take eyes off compliance at higher levels. Busy managers and senior managers can also be guilty of taking shortcuts with compliance or ignoring non-compliant activities because they do not have the time to “sort it out” – when, in truth, the failure to take action is a failure of management.
Also Visit: Considered PHI Under HIPAA
Step 6: The Best Sanctions are Not Always Disciplinary
Sanctions policies can often be overwhelming documents threatening all manner of disciplinary actions for non-compliance from warnings to suspensions, to termination of contract and loss of license. Some even include the maximum federal penalties for violations of §1177 of the Social Security Act (up to ten years in prison and up to $250,000 in fines).
Although these sanctions may have to legally be included in a sanctions policy, making them the focus of attention is not necessarily the best way to cultivate a culture of compliance. The threat of a loved one being the victim of medical identity theft and the consequences of data breaches can encourage workforce compliance more than the threat of refresher training.
Step 7: Responding Quickly is the Key to Compliance
One of the keys to cultivating a culture of compliance is to respond to queries, issues, complaints, reports of violations, and data breaches as quickly as possible. Responding quickly to any type of communication demonstrates a commitment to compliance and an eagerness to ensure – once a compliant workforce is achieved – the compliant state is maintained.
Responding to queries, issues, complaints, etc. would ordinarily be the responsibility of compliance officers (or teams), but this can lead to the compliance officers being overwhelmed. Consequently, it may be necessary for managers and senior managers to take some responsibility for monitoring compliance and responding to workforce or patient communications.
